The Diabetes Dictionary: Decode Blood Sugar Relevant Terms & Tests, HbA1c, OGTT & More | Redcliffe Labs

Medically Reviewed By
Dr. Neha Prabhakar
Written By Komal Daryani
on Nov 13, 2025
Last Edit Made By Komal Daryani
on Nov 14, 2025

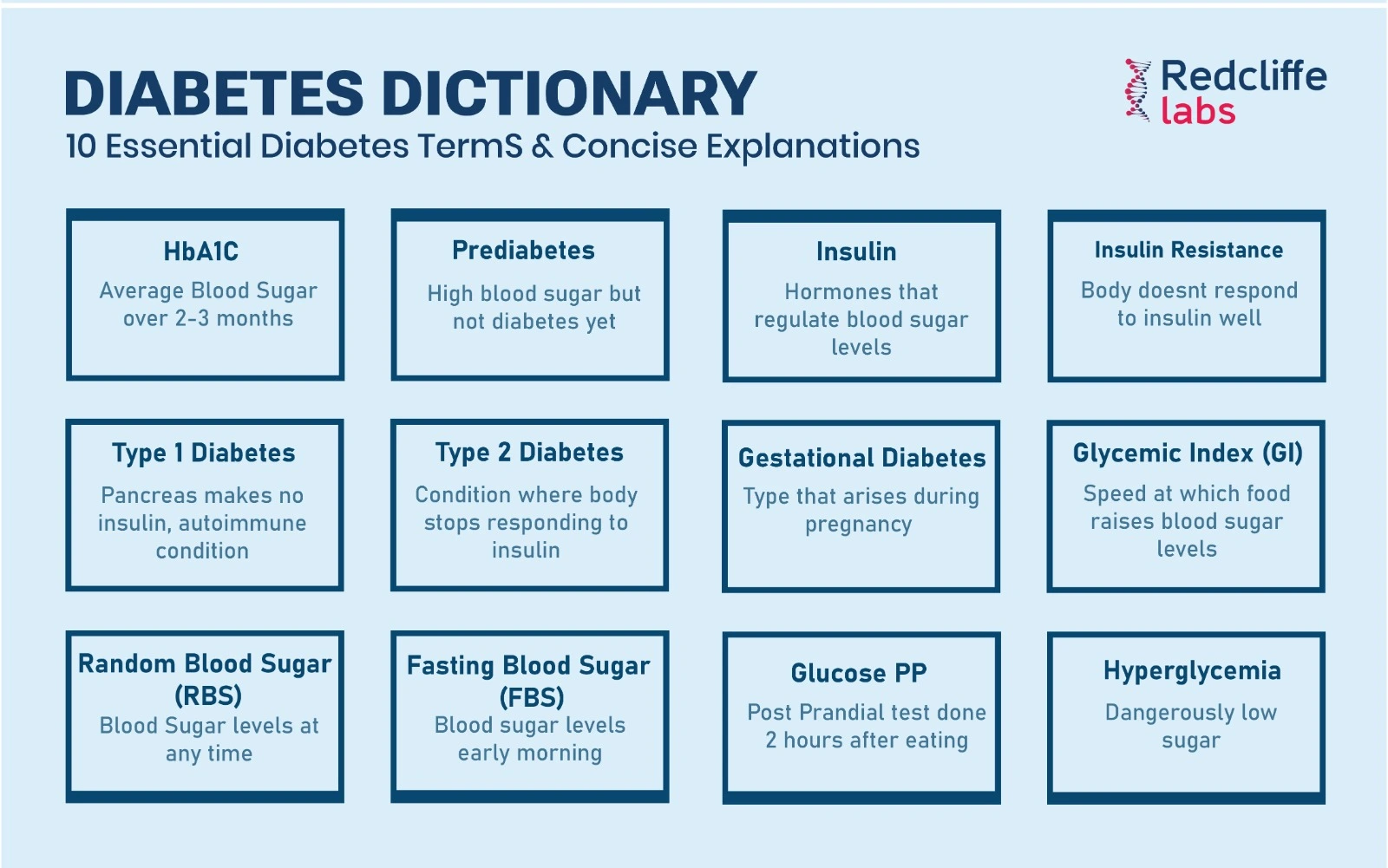
Understanding the terms and numbers in blood sugar test reports is not just a matter of curiosity, but a practical skill that empowers you in clinical conversations, helps you select the right tests, and enables earlier, more informed decisions about prevention and treatment. This guide is here to help you gain this understanding and take control of your health.
This guide decodes the most common diabetes-related laboratory terms, including fasting plasma glucose (FPG) and postprandial glucose, as well as HbA1c and C-peptide. It explains what each result means in plain clinical language, how tests are used in diagnosis and monitoring, and which combinations of results are most significant.
This guide is designed to be a practical reference, shared by highly experienced medical professionals, that you can use when you receive your next diabetes report, or for a detailed discussion with your clinician, or to exactly understand what the medical report of your family member indicates. It's here to reassure you that you have the tools you need to navigate these reports with confidence.
The clarity of the medical jargon related to diabetes is as important as understanding the Gen Z slang.
Before jumping into the Diabetes Dictionary, let's start with the basics
What is Diabetes?
Diabetes mellitus is a group of metabolic disorders characterized by chronically elevated blood glucose due to defects in insulin secretion, insulin action, or both.
Insulin is the hormone that enables glucose to move from the bloodstream into cells for energy. When this system fails, glucose accumulates in the blood, and chronic hyperglycemia increases the risk of vascular, renal, neurological, and ocular complications.
The principal clinical aims in diabetes management are early detection, accurate classification of diabetes type, and regular monitoring. These steps are crucial in preventing complications, and laboratory tests play a central role in each of them.
Types of Diabetes: Clinical overview with practical implications
- Type 1 diabetes. An autoimmune destruction of pancreatic beta cells leads to near-absolute insulin deficiency. It generally presents in children and young adults but can occur at any age. Patients with type 1 require insulin replacement and monitoring for acute metabolic complications such as diabetic ketoacidosis.
- Type 2 diabetes. Characterized by insulin resistance with a relative insulin secretory defect. It is strongly associated with overweight, a sedentary lifestyle, and specific dietary patterns. Many cases can be delayed or managed initially with lifestyle change and oral therapy; however, progressive beta-cell dysfunction can necessitate insulin therapy.
- Gestational diabetes. Glucose intolerance with onset or first recognition during pregnancy. It requires close monitoring because it affects both maternal and fetal outcomes and increases the lifetime risk of Type 2 diabetes for the mother.
- Prediabetes. A state in which blood glucose values are above normal but below the threshold for diabetes. Prediabetes is clinically significant because it is a reversible phase where lifestyle and therapeutic interventions reduce progression to diabetes.
Each of these categories has different diagnostic thresholds and different test preferences, which are discussed below.
Diabetes Dictionary: That defines core blood sugar tests and what each measures
-
Fasting Plasma Glucose (FPG): the baseline metabolic snapshot
FPG measures blood glucose after at least eight hours of fasting and reflects the body's ability to maintain a stable baseline glycemia. It is widely used as a screening and diagnostic test because the procedure is simple and reproducible.
Diagnostic or Report References (typical clinical cutoffs):
- Normal: FPG < 100 mg/dL
- Prediabetes: FPG 100–125 mg/dL
- Diabetes: FPG ≥ 126 mg/dL (confirmed on a separate day or with another diagnostic test)
Clinically, elevated FPG suggests impaired basal glucose regulation, often due to hepatic glucose overproduction and declining insulin secretion.
-
Postprandial Blood Sugar (PPBS): The after-meal test
PPBS measures glucose typically two hours after a standard meal and assesses how the body handles the glucose load from food. Elevated postprandial values can persist even when fasting glucose levels are normal, providing critical information about early insulin secretory defects or insulin resistance.
Common clinical interpretation:
- Normal: < 140 mg/dL (2-hour value)
- Impaired glucose tolerance: 140–199 mg/dL
- Diabetes: ≥ 200 mg/dL
A persistently high PPBS is strongly associated with cardiovascular risk and is therefore clinically meaningful even when fasting values are acceptable.
-
HbA1c (Glycated Hemoglobin): The three-month average
HbA1c measures the proportion of hemoglobin that has glucose attached; because red blood cells have an average lifespan of about three months, HbA1c reflects average glycemia over that period. It is used both to diagnose diabetes and to monitor long-term glycemic control.
Guideline ranges commonly used:
- Normal: < 5.7%
- Prediabetes: 5.7–6.4%
- Diabetes: ≥ 6.5%
Practically, HbA1c is less sensitive to short daily fluctuations and is especially useful for assessing long-term control and response to treatment. Conditions that alter red cell turnover (hemolytic anemia, recent transfusion) can interfere with HbA1c interpretation and require alternative measures.
-
Oral Glucose Tolerance Test (OGTT): The metabolic challenge
The OGTT involves fasting, ingestion of a standardized glucose drink (commonly 75 g in adults), and serial blood sampling, usually with a key measurement at two hours. The OGTT evaluates the dynamic ability of the body to clear a glucose load and is the preferred test for diagnosing gestational diabetes and for uncovering impaired glucose tolerance that fasting tests may miss.
Two-hour thresholds (common):
- Normal: < 140 mg/dL
- Impaired tolerance: 140–199 mg/dL
- Diabetes: ≥ 200 mg/dL
OGTT is more sensitive than fasting glucose in certain populations and is often used when clinical suspicion remains despite normal fasting glucose levels.
-
Insulin assay: Looking behind the glucose numbers
Measuring fasting and stimulated insulin levels helps differentiate between insulin deficiency and insulin resistance. Elevated insulin levels despite elevated glucose indicate insulin resistance; low or absent insulin levels with hyperglycemia suggest deficient insulin production. This information can help clinicians decide between insulin sensitizers, secretagogues, or direct insulin replacement.
-
C-peptide: An index of endogenous insulin production
C-peptide is co-secreted with insulin in equimolar amounts and serves as a reliable marker of the body's endogenous insulin production. It is clinically valuable for:
- Distinguish between Type 1 and Type 2 diabetes in unclear cases
- Evaluate residual beta-cell function when considering insulin therapy.
- Assess the causes of hypoglycemia related to insulin production or exogenous insulin.
Low C-peptide levels in the presence of hyperglycemia indicate low endogenous insulin production, as seen in Type 1 diabetes; high or normal C-peptide levels with hyperglycemia suggest insulin resistance.
-
Random Blood Sugar (RBS): Convenience screening
RBS is a convenient measurement that can be taken at any time of day. Isolated high values require confirmation, but an RBS ≥ 200 mg/dL in a patient with classic symptoms of diabetes (polyuria, polydipsia, unexplained weight loss) is strongly suggestive of diabetes.
Disclaimer: The values mentioned above are standard reference ranges and may vary across laboratories due to differences in equipment calibration and testing methods. Please refer to the reference ranges provided in your lab report for accurate interpretation.
How to interpret combinations of test results?
Usually, the diabetes result patterns appear in the reports in the below-mentioned format, and here's what they most often indicate:
- High FPG + high PPBS: Consistent impaired glucose regulation both at baseline and after meals; likely established diabetes requiring a full management plan.
- Normal FPG + elevated HbA1c: Suggests that daily or postprandial hyperglycemia is contributing to an increased average; ask about lifestyle and consider post-meal testing or continuous glucose monitoring.
- High 2-hour OGTT with normal FPG: Early glucose intolerance that fasting tests miss; common in impaired glucose tolerance and pregnancy.
- High insulin with high glucose: Functional insulin resistance; clinical management focuses on weight reduction, exercise, and insulin-sensitizing agents.
- Low C-peptide with high glucose: Minimal endogenous insulin production; often indicates Type 1 diabetes or advanced beta cell failure.
Clinicians make diagnostic and management decisions by reviewing laboratory results in conjunction with the clinical history, physical examination, and, when necessary, imaging or antibody testing.
Practical table: commonly used diagnostic thresholds (for quick reference)
|
Test |
Normal |
Prediabetes / Impaired |
Diabetes (diagnostic) |
|
Fasting Plasma Glucose (mg/dL) |
< 100 |
100–125 |
≥ 126 (on 2 occasions or with confirmatory test) |
|
2-hour OGTT (mg/dL) |
< 140 |
140–199 |
≥ 200 |
|
HbA1c (%) |
< 5.7 |
5.7–6.4 |
≥ 6.5 |
|
Random Plasma Glucose (mg/dL) |
— |
— |
≥ 200 with symptoms |
Note: These thresholds are widely used in clinical practice. Local guidelines may vary slightly, and clinicians interpret results within the full clinical context.
Common pitfalls and test-specific caveats clinicians watch for
- HbA1c limitations. Hemoglobin variants, anemia, recent blood transfusions, or conditions that alter red cell lifespan can yield misleading HbA1c values; alternative assessments, such as fructosamine, may be considered.
- OGTT reproducibility. OGTT preparation and timing can significantly affect results; improper fasting, recent illness, or certain medications can alter the outcome.
- Insulin/C-peptide assays. Assay standardization and reference ranges vary; clinical interpretation must consider local lab calibration.
- Single high value. A single abnormal result often requires confirmation when making a diagnosis; clinical symptoms and multiple tests guide the conclusions.
Lifestyle and clinical actions that follow from common test results
- Prediabetes: Intensive lifestyle intervention (dietary change, regular physical activity, weight loss) is the first-line approach and can prevent progression. Pharmacologic therapy is considered in high-risk individuals.
- Newly diagnosed Type 2 diabetes: Initial care includes individualized lifestyle modification, glycemic monitoring, and a choice of glucose-lowering agents based on comorbidities and risk. Education and complication screening are initiated.
- Type 1 diabetes: Immediate initiation of insulin therapy and patient/caregiver education on insulin administration, hypoglycemia recognition, and sick-day management are essential.
- Gestational diabetes: Tight glucose control during pregnancy, fetal monitoring, and postpartum screening are required.
Timely laboratory follow-up and coordination with the treating clinician ensure appropriate therapeutic choices.
You May Also Read: https://redcliffelabs.com/myhealth/diabetes/vitamin-deficiencies-in-diabetes/
Nutrition note: Glycemic index, meal composition, and testing relevance
Understanding how foods affect blood sugar is practical and actionable. The glycemic index classifies carbohydrates by their effect on blood glucose; choosing low-GI, high-fiber foods reduces postprandial spikes and supports better HbA1c outcomes. Meal composition (protein, fiber, healthy fats) slows glucose absorption and mitigates rapid rises observed in PPBS or OGTT.
How Redcliffe Labs supports accurate diabetes diagnosis and monitoring
At Redcliffe Labs, we offer validated laboratory assays for FPG, PPBS, OGTT, HbA1c, insulin, and C-peptide, providing clinically relevant reporting and clinician-verified interpretations. We aim to pair technical accuracy with clear explanations of results so that patients can understand the implications and next steps. For questions about your specific result, request a clinician-reviewed interpretation or consult your treating physician.
Final takeaways:
- Single numbers should be interpreted within the clinical context; patterns are more important than isolated values.
- HbA1c gives a longer-term picture; FPG and PPBS/OGTT provide immediate state information.
- C-peptide and insulin assays help determine the cause, whether it is low production or resistance.
- Prediabetes is reversible; early action prevents progression.
- Discuss your complete report with your clinician and ask which tests are most suitable for your situation.
If you would like a clinician review of your blood sugar report or want to book diabetes-specific tests (FPG, OGTT, HbA1c, insulin, C-peptide) with home sample collection, Redcliffe Labs is available nationwide. Book a test online or call our helpline to request a report review from one of our laboratory consultants.
Frequently Asked Questions (FAQs)
Q: Which test should I get first if I'm worried about diabetes?
A: For general screening, fasting plasma glucose and HbA1c are commonly used because they are simple and informative. If results are borderline or symptoms persist, an OGTT or postprandial testing may be advised.
Q: Can HbA1c change quickly after lifestyle improvements?
A: HbA1c reflects average glycemia over approximately three months; meaningful changes are usually detectable after six to twelve weeks of sustained intervention.
Q: Does stress or illness affect my glucose tests?
A: Yes. Acute illness, infection, recent surgery, certain medications, and stress hormones can transiently raise glucose values and affect test interpretation.
Q: Is OGTT necessary for pregnancy screening?
A: OGTT is frequently recommended between 24 and 28 weeks of pregnancy to screen for gestational diabetes, as it is more sensitive than fasting glucose alone in that setting.
Q: When should C-peptide be measured?
A: C-peptide is measured when clinicians need to determine endogenous insulin production, particularly in cases where the type of diabetes is unclear or when planning treatment transitions.



